Blog
Nursing Leadership Challenges for The Care of Older Patient with Dementia
Background of the Study
Ageing is a significant risk factor for neurodegenerative diseases, including dementia, making them more vulnerable to hospital admissions than other age groups, occupying at least two-thirds of the acute hospital beds (Cantón-Habas et al., 2020). Dementia is a clinical syndrome characterised by acquired loss of emotional and cognitive capabilities severe enough to limit an individual’s daily functioning and quality of life (Suzuki et al., 2019). The incidence of dementia among the elderly population is rapidly increasing globally. There are different subtypes of dementia, which include Alzheimer’s disease (AD), vascular dementia, mixed dementia, Parkinson’s disease, Huntington’s disease, dementia with Lewy bodies, Creutzfeldt-Jacob disease, normal pressure hydrocephalus, frontotemporal dementia/Pick’s disease (Cantón-Habas et al., 2020). However, AD is the common subtype of dementia, affecting about half of dementia patients. According to the World Health Organisation (WHO) (2021), at least 55 million people live with dementia globally, with more than 60% of these patients coming from low- and middle-income countries. Furthermore, at least 10 million new cases of dementia are reported yearly (WHO, 2021). Significant risk factors for dementia include ageing, hypertension, diabetes, obesity and overweight, smoking, alcoholism, depression, social isolation and physical inactivity (Suzuki et al., 2019). Even though dementia does not affect consciousness, it leads to cognitive function impairment, occasionally preceded by changes in emotional control, mood, behaviours and motivation.
Systematic Literature Review Writing Services
Maximize your research impact with our tailored systematic literature reviews writing services. Let our experts help you craft a comprehensive, structured review that elevates your work to the next level!
Nurse leadership is the ability of a nurse leader to influence, inspire and motivate other care professionals as they collaboratively work together to realise their goals (Kelly, Lefton, and Fischer, 2019). Core competencies for nurse leaders include communication and relationship, knowledge of the healthcare environment, management, professionalism, leadership, and business skills and principles (Flaherty and Bartels, 2019). As reported by Kelly, Lefton and Fischer (2019), nurse leaders are involved in creating novel care models and new workflows to accommodate and address the increasing demands for managing patients’ needs in contemporary healthcare settings. According to Hofmeyer and Taylor (2021), nurse leaders are actively involved in the provision of quality and safe care services to older patients by upholding older patients’ right to respect, dignity and autonomy, contributing to clinical governance systems, participating in the decision-making processes consistent with their values and goals, and delivery of safe, quality care irrespective of the care environment. Nurse leaders are vital members of the clinical governance systems who contribute significantly to monitoring, measuring and improving the safety, quality and appropriateness of clinical care services offered to older patients (Flaherty and Bartels, 2019). Care needs for older people often vary depending on the involved care environment and presenting health problems (Hofmeyer and Taylor, 2021). Therefore, nurse leaders work collaboratively with other care professionals and families to personalise care models for older people to meet their expressed needs.
Evidence from the existing studies by de Oliveira et al. (2019) and Şahin, Özer, and Yanardağ (2019) shows that the quality of care provided to older patients is greatly influenced by the perspectives of the care providers, including nurses. Therefore, the behaviours and knowledge of nurses often influence their preferences for caring for older patients, affecting the overall quality of care they offer. The attitude of nurses towards older patients is among the most critical factors influencing the quality of care provided to this population. For example, an analysis by Karaca and Durna (2019) reports that nurses who demonstrated patience and respect towards older patients because of their age could adequately pay attention to their needs and prioritise their care over other age groups. Similarly, the study by Molina-Mula and Gallo-Estrada (2020) establishes that nurses who have negative attitudes towards older patients are often unable to address the care needs of this population. Furthermore, the study by Palati et al. (2020) identifies a lack of special facilities within the hospital to care for older patients and a lack of motivation among nurses who believe that caring for older patients is time-consuming as other vital factors limiting successful care management of older patients, including those with dementia. Consistent findings are reported in the previous analyses by Landeiro et al. (2019) and Şahin, Özer, and Yanardağ (2019), which establish that lack of social support for older patients, limited or complete lack of clear health policies for older patients, low-skill and competency levels among nurses in gerontology as other vital factors undermining care for older patients. Therefore, nurse leaders should develop new strategies for addressing the challenges and care issues for older patients, specifically those with dementia.
Research Aim
To identify nurse leadership strategies that improve care for older patients with dementia.
Research Objectives
- To identify and critique the care issues that create care delivery difficulties for nurses caring for older patients with dementia.
- To identify and critique nurse leadership strategies that contribute to and alleviate care difficulties arising from older patients with dementia.
- To critically examine wider care contexts, including policies, practices and care philosophies, that may assist in reducing care issues for older patients with dementia.
Methods
Search Strategy and Databases
A systematic literature review (SLR) was adopted in this study to facilitate the identification and critical appraisal of evidence from the existing literature about the challenges experienced by nurse leaders in caring for older patients with dementia. According to Mengist, Soromessa, and Legese (2020), SLR involves identifying, selecting and critically evaluating research to generate new knowledge to answer the formulated research question. A literature search was conducted on three databases: CINAHL, PsycINFO and PubMed (Medline). Their high reputations influenced the selection of these databases in hosting up-to-date and top-quality nursing and human health literature. The keywords and search terms used during the literature search process include “nurse” OR “nursing leadership” OR “nurse leader” AND “challenges” OR “issues” OR “experiences” AND “older patients” OR “ageing patients” OR “geriatric patients” AND “dementia” OR “Alzheimer’s disease” OR “Parkinson’s disease”.
Eligibility Criteria
Inclusion criteria
The first inclusion criterion applied during the literature search process was based on the overall aim of the study, where only those studies which assessed nurse’s leadership challenges in the care of older patients with dementia were included. This criterion was vital in ensuring the homogeneity of the collected evidence for review and generated findings from the literature synthesis. Furthermore, the literature search was limited to only primary qualitative or mixed methods studies. Publication characteristics of the studies were also applied during the literature search process. Precisely, only those studies published initially in English and in 2013-2023 were selected for review. Including studies published within the last ten years was appropriate for ensuring the selection and inclusion of up-to-date information about the challenges nurses face when caring for older patients with dementia.
Exclusion criteria
Studies that assessed other health issues experienced by older patients apart from dementia were excluded during the literature search. Furthermore, all the studies published before 2013 and in other languages apart from English were eliminated. The literature search strategy was further set to eliminate primary quantitative studies or secondary studies such as meta-analyses and systematic reviews. Studies not related to nursing leaders caring for older patients with dementia were also eliminated. A complete description of the eligibility criteria applied during the literature search is presented in Table 1 below.
Table 1: Description of eligibility criteria
| Factor | Inclusion Criteria | Exclusion Criteria |
| Research aim | Nurse’s leadership challenges in the care of older patients with dementia | Issues experienced by nurses caring for other populations other than dementia patients |
| Population of interest | Older patients (>65 years old) with dementia | Patients <65 years old Non-dementia older patients |
| Publication data | 2013-2023 | 2012 and earlier |
| Publication language | English | Other languages apart from English |
| Study type | Primary qualitative studies or mixed-methods studies | Primary quantitative studies, secondary studies such as systematic reviews and meta-analyses |
Critical/Quality Appraisal
The quality of studies selected for this review was assessed using the Critical Appraisal Skill Programme (CASP) checklist for qualitative studies. The CASP checklist for qualitative studies comprises ten questions, which allow the reviewer to systematically criticise evidence presented in the individual studies (CASP, 2018). Each question has a maximum award of 1 point and a minimum of 0 points. The first two questions are screening questions, and only those studies that record “Yes” or a maximum of 2 points would proceed to the following quality appraisal stage. Precisely, a “Yes” response is “1 Point” while “Cannot Tell” or “No” is “0 Point”. Only studies which recorded 8-10 points were selected for review. Results from the quality assessment process using CASP are presented in Appendix 2.
Analysis
Relevant data from the selected studies were extracted for further analysis and interpretation. The collected data are presented in the literature matrix, Appendix 1. The collected data were organised in the literature matrix table to synthesise evidence from the selected studies and draw meaningful conclusions. After that, a thematic analysis approach was used for analysing the collected data to generate key themes about the challenges experienced by nurses when caring for older adults with dementia. According to Clarke and Braun (2021), thematic analysis allows for the documentation, scrutiny, and construal of critical patterns of meaning within the qualitative data. The themes generated from thematic analysis include factors influencing care delivery challenges, nurse leadership strategies for enhancing care delivery, and care policies and philosophies for reducing care issues.
Literature Search Results
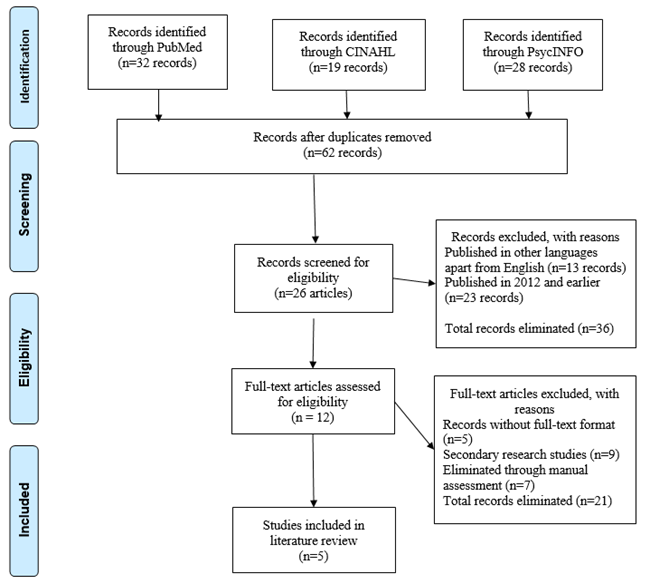
The initial literature search process on the three databases led to the identification of 79 recordings, which were further subjected to eligibility assessment to facilitate selecting the most appropriate ones for review. All the duplicates were removed, and a total of 17 recordings were eliminated. An additional 36 recordings were eliminated for different reasons: 23 were published in 2012 and earlier, while 13 were published in languages other than English. Furthermore, 14 publications were eliminated from the remaining 26 recordings for different reasons: 5 papers without full-text format and 9 secondary research-based papers. After that, the remaining 12 full-text publications were subjected to manual quality assessment, where 7 studies were excluded. The remaining 5 full-text publications were included in this SLR. The PRISMA diagram below presents a detailed description of the literature selection process.
Figure 1: PRISMA Diagram Showing the Literature Selection Process
Findings
Characteristics of The Selected Studies
Four of the five studies included in this review were primary qualitative research, while Piirainen et al. (2021) adopted mixed-methods research. However, only the qualitative results presented in the study by Piirainen et al. (2021) were extracted and included in the present review. Furthermore, different qualitative research designs were implemented in these studies. While Fukuda, Shimizu and Seto (2015) used only a focus group discussion in their analysis, Sagbakken, Spilker, and Nielsen (2018) adopted both in-depth interviews and focus group discussions, hence making data collected for analysis in the latter to be more comprehensive than the former. Furthermore, Dookhy and Daly (2021) employed a qualitative descriptive design to understand the challenges experienced by nurses when caring for older patients with dementia. On the other hand, Pennbrant et al. (2020) implemented a phenomenological research design involving nine semi-structured interviews with nurses in palliative care settings.
Research settings for the studies included in this review varied among the five studies. For example, the studies by Dookhy and Daly (2021) and Fukuda, Shimizu and Seto (2015) were conducted in acute care settings involving the treatment of comorbidities among dementia patients. Furthermore, the study by Pennbrant et al. (2020) was conducted in residential aged-care units where palliative care services were provided to older patients with dementia. On the other hand, the study by Piirainen et al. (2021) was conducted in two nursing homes, while the research by Sagbakken, Spilker and Nielsen (2018) was performed in dementia care units within the selected hospitals. Including studies conducted in different health settings was appropriate for ensuring the comprehensiveness of the collected for analysis. Contrary to the other four studies, which only collected data from the nurses and other care practitioners, the study by Sagbakken, Spilker and Nielsen (2018) also included perceptions of dementia patients and their families regarding the quality of care they receive from the nurses.
Generated Themes
Theme 1: Factors Influencing Care Delivery Challenges
The first theme comprised the primary factors influencing the development of challenges experienced by nurses caring for older patients with dementia. All five studies included in this review presented different factors associated with negative experiences among nurses. However, a comparative assessment of evidence from the five studies shows that even though nurses often seek to understand the reasoning associated with responsible behaviours, they are greatly challenged by the environmental, emotional, organisational and educational challenges that are linked with the care experiences when caring for older patients with dementia. Analysis by Dookhy and Daly (2021) identifies factors such as frequent movement of dementia patients within the care setting and unfamiliar environment as crucial factors that increase levels of disorientation among this patient population and that such challenges were stressful to be with dementia.
The study by Fukuda, Shimizu and Seto (2015) established that most nurses are often challenged by the physical design and layout of the ward environment where the dementia patients are treated, specifically when trying to develop a more familiar environment for addressing responsive behaviours among their clients. A similar challenge has been reported in the study by Pennbrant et al. (2020), which associated its development with the fact that most dementia patients often share care settings with other patient populations, limiting the successful implementation of the tailored care approach.
Evidence from the studies by Piirainen et al. (2021) and Fukuda, Shimizu and Seto (2015) shows that problematic patient behaviours influence negative experiences among nurses caring for dementia patients. Precisely, Fukuda, Shimizu and Seto (2015) noted that continuous changes in the care environment, anxiety among dementia patients, physical restrictions and painful treatments influenced the development of problematic patient behaviours. On the other hand, the study by Sagbakken, Spilker and Nielsen (2018) reported unfamiliarity with the test situations, lack of continuity and poor information exchange in the chain of care as critical challenges that limited the ability of nurses to provide quality care to older patients with dementia.
Theme 2: Nurse Leadership Strategies for Enhancing Care Delivery
The second theme was developed using evidence about the strategies nurse leadership can use to address the challenges and improve the quality of care delivered to older patients with dementia. Two studies, Dookhy and Daly (2021) and Pennbrant et al. (2020) identified the development of specialised knowledge and skills as an essential strategy that nurse leaders and all members of the nursing team should adopt in order to address the challenges they experience when caring for older patients with dementia. According to Dookhy and Daly (2021), work experience among nurses enhances their ability to develop specialised knowledge and skills, while inadequate knowledge and skills influence the development of insecurities in their professional roles. The study by Pennbrant et al. (2020) further reported that through developed specialised knowledge and skills, nurses caring for dementia patients can understand and interpret dementia patients’ expressions precisely when behavioural disorders are involved.
Another strategy reported in three studies, Pennbrant et al. (2020), Piirainen et al. (2021) and Sagbakken, Spilker and Nielsen (2018), is the adoption of teamwork as a work standard. As stated by Pennbrant et al. (2020), the ability of nurse leaders to supervise the care delivery process helps empower and motivate the entire nursing team to deliver quality care. A substantial part of the nurse leaders’ work should involve supporting nurse assistants to understand and interpret all the needs of older patients with dementia. Piirainen et al. (2021) further identified knowledge sharing as an essential part of the nursing teamwork cooperation when caring for dementia patients. Consistent findings are reported in the study by Sagbakken, Spilker and Nielsen (2018), which established that working in teams where all the involved care professionals can provide their perceptions about the older patients’ care needs may help create conditions for safe and high-quality care.
Two studies, Fukuda, Shimizu and Seto (2015) and Pennbrant et al. (2020), identified creating positive relationships with dementia patients as another essential strategy nurse leaders can use to enhance the quality of care and address the challenges they experience. Specifically, Fukuda, Shimizu and Seto (2015) stressed the need for nurses caring for older dementia patients to know their clients personally and understand their needs and resources, making them feel safe and calm during the care process. Similarly, Pennbrant et al. (2020) reported that care conditions may be problematic if older patients with dementia do not understand nurses’ intentions, possibly leading to problematic behaviours. According to Pennbrant et al. (2020), nurse leaders can create positive relationships with their dementia patients by inviting patient’s families to be part of the treatment process. Including family in the treatment process allows nurse leaders to acquire more information about older patients with dementia, hence effectively addressing their needs.
Theme 3: Care Policies and Philosophies for Reducing Care Issues
The third theme comprised evidence about the care contexts, including policies, practices and care philosophies, that may assist in reducing care issues for older patients with dementia. The first care policy reported in this review involved enhanced continuity of care. According to Dookhy and Daly (2021) and Sagbakken, Spilker and Nielsen (2018), most nurses often face many challenges when caring for dementia patients because the health organisations in which they work do not have appropriate mechanisms for ensuring continuity of care, right from the admission point to the discharge. Furthermore, results from the analysis by Sagbakken, Spilker and Nielsen (2018) show that developing a treatment programme that focuses on ensuring that dementia patients seek treatment from the same care personnel improves care outcomes. Evidence from both studies shows that older patients with dementia with high continuity of care often receive high-quality care compared to those seeking dementia-related care from different practitioners.
Find the attached PDF version of this Systematic Review Example
The other care policy reported in the reviewed studies is improved information exchange in the care chain. The studies by Dookhy and Daly (2021) and Sagbakken, Spilker and Nielsen (2018) established that the concept of sharing dementia patients’ vital information securely with other care practitioners within the care team helps in improving the speed, safety, quality and cost of patient care. Similarly, an analysis by Pennbrant et al. (2020) reported that effective collaboration among nurses and other members of the nursing team caring for older patients with dementia often requires adequate information exchange during the transition within the chain of care, continually among the care professionals as well as a shared understanding of the goals for treatment and care. Furthermore, Piirainen et al. (2021) and Sagbakken, Spilker and Nielsen (2018) recommended the adoption of dementia support systems within the healthcare organisation tasked with providing information and advice about dementia. Improved information exchange in the chain of care helps enhance the quality of care provided to dementia patients and reduces the severity of challenges experienced by nurses when caring for older patients with dementia.
Discussion
The first objective of this review was to identify and critique the care issues that create care delivery difficulties for nurses caring for older patients with dementia. Generally, most of the challenges experienced by nurses in dementia care settings are influenced by problematic behaviours among the patients. The review established that nurses are required to deal with problematic patient behaviours. Precisely, the studies by Fukuda, Shimizu and Seto (2015) and Sagbakken, Spilker and Nielsen (2018) reported that nurses are often required to take measures such as placing sensor mats and hiding intravenous infusion lines in order to prevent the occurrence of problematic behaviours among the dementia patients. Nonetheless, a previous study by Cantón-Habas et al. (2020) established that incorporating new strategies into the care plan may make the environment less familiar to dementia patients, leading to more advanced problematic behaviours. Consistent with the evidence from the previous analysis by Suzuki et al. (2019), the present review has further established that environmental stimulation may exaggerate stress response among patients with dementia. Therefore, dementia patients and their families should be aware of any change in the care environment.
The present review has further established that a significant number of challenges experienced by nurses caring for dementia patients are influenced by factors such as the physical design and layout of the ward environment where the dementia patients are treated and unfamiliarity with the test situations. Results from this review are further supported by the empirical evidence from the previous analyses by Oliveira et al. (2019) and Şahin, Özer and Yanardağ (2019), which identified the composition of the physical environment of dementia treatment setting as a significant concern. Precisely, the studies by Dookhy and Daly (2021) and Pennbrant et al. (2020) recommended incorporating dementia-inclusive design principles at both the word and organisational levels to enhance the quality of care provided to dementia patients. Evidence synthesised in this review, specifically data from the studies by Fukuda, Shimizu and Seto (2015) and Piirainen et al. (2021), demonstrated that noisy, unfamiliar, and fast-paced ward and hospital environments influence the occurrence of high incidences of responsive behaviours among older dementia patients. Therefore, the treatment environments should be conducive for older patients with dementia to reduce the severity of challenges experienced by the nurses caring for such patients.
The second objective of this review was to identify and critique nurse leadership strategies that contribute to and alleviate care difficulties arising from older patients with dementia. Results from the conducted analysis showed that different strategies can be used to address challenges experienced by nurses caring for older dementia patients. The reported strategies in this context include the development of specialised knowledge and skill frameworks, adopting teamwork as a work standard, and creating positive relationships with dementia patients. Previous analysis by Molina-Mula and Gallo-Estrada (2020) reported that most nurses face many challenges when providing palliative care because they need more knowledge and skills to interpret and understand the needs of their patient populations. Results from some of the studies included in this review, such as Piirainen et al. (2021) and Sagbakken, Spilker and Nielsen (2018), show that most nurses often depend on their work experience to understand the needs of their clients with dementia and to seek knowledge about palliative care in dementia management continually. Generally, most nurses face many challenges when caring for dementia patients because of their inability to understand and interpret the care needs of this patient population. This review has also stressed the need for nurse leaders to adopt teamwork as a working method and enhance the relationship between the nursing team and dementia patients. Precisely, evidence from the studies by Fukuda, Shimizu and Seto (2015) and Piirainen et al. (2021), which is also supported by those from the previous analyses by de Oliveira et al. (2019) and Şahin, Özer and Yanardağ (2019) shows that collaboration with other care professionals is essential for providing quality care to the older patients with dementia. The multidisciplinary teams for dementia management should include the care professionals, dementia patients and their families for adequate care provision.
The third objective of this review was to critically examine broader care contexts, including policies, practices and philosophies, that may assist in reducing care issues for older patients with dementia. Precisely, two care policies were reported in this review: enhanced continuity of care and improved information exchange in the care chain. Results from this review showed that continuity of care is an essential strategy for enhancing the quality of care services offered to older adults with dementia. According to Piirainen et al. (2021) and Pennbrant et al. (2020), there is a need to develop a clear care plan and unambiguous support structures to ensure the continuity of palliative care offered to older patients with dementia. Even though the present review stressed the importance of multidisciplinary teams and care plans, previous analyses by Landeiro et al. (2019) and Şahin, Özer and Yanardağ (2019) established that it is often challenging to make a prognosis for older patients with dementia and that deaths may not be accurately predicted. Through continuity of care, patients can receive dementia care from a specific health practitioner with advanced knowledge and experience about their care needs, improving their quality of life. Results from the present review, precisely evidence from the studies by Sagbakken, Spilker and Nielsen (2018) and Dookhy and Daly (2021), demonstrated that a significant number of the challenges experienced by nurses caring for dementia patients are caused by poor information exchange in the care chain. Therefore, this review recommended enhancing the quality of information exchange in the care chain to ensure improved quality of care offered to older patients with dementia.
Conclusion and Recommendations
Conclusion
The primary aim of this review was to identify nurse leadership strategies that improve care for older patients with dementia. From a general perspective, the present review has established that nurses’ experience is often influenced by the environmental, emotional, organisational and educational challenges linked with the care experiences when caring for older patients with dementia. Different strategies for addressing challenges experienced by nurses when caring for older dementia patients have been reported in the present review. The first approach involves the development of a specialised knowledge and skill system, which helps enhance nurses’ competency levels. Furthermore, this review has identified the adoption of a teamwork approach as a work standard within the dementia care programme as a critical strategy for involving all nursing team members to ensure improved quality of care offered to dementia patients. Nurse leaders should supervise the delivery process to empower and motivate other nursing team members to deliver quality care to dementia patients. The review has also identified creating a positive relationship between patients and the nursing team as a critical strategy for addressing challenges experienced by nurses caring for dementia patients. At the care context level, this review identified enhanced continuity of care and improved information exchange in the care chain as other essential strategies for addressing challenges experienced in nursing caring for dementia patients.
Limitations of the Review
The present review assessed challenges experienced by nurses caring for dementia patients in general without accounting for the fact that different dementia patients have varying care needs and associated challenges when caring for them. Therefore, future reviews in this context should focus on assessing challenges experienced by nurses caring for specific groups of dementia patients, including AD, vascular dementia, and Parkinson’s disease, among others. Furthermore, this review included studies from different care settings, such as residential homes and intensive care units; the reported findings could not be applied within a specific healthcare context. Dementia patients in residential care homes and intensive care units might have different care needs. Therefore, future research should focus on including only dementia patients from specific care settings, such as residential care homes.
Recommendations for Practice
Newly generated knowledge from the present review has important implications for the nursing care practice for older patients with dementia. Specifically, the present review has established the need for health facilities caring for older dementia patients to adopt continuity of care to improve the quality of care services offered to this patient population. Additionally, dementia care facilities should have enhanced information exchange systems in their care chain to ensure that the health needs of dementia patients are adequately addressed. Adoption and implementation of dementia support systems are also recommended to improve the quality of care offered to older patients. The conducted review further established that most of the challenges experienced by nurses caring for dementia patients are associated with the patients’ problematic behaviours. Therefore, nurse leadership should address all the factors that lead to problematic behaviours among older dementia patients. The problems to be addressed for improved care experience among dementia nurses include frequent movement of dementia patients within the care setting and unfamiliar environment, physical design and layout of the ward environment.
References
- Cantón-Habas, V., Rich-Ruiz, M., Romero-Saldaña, M. and Carrera-Gonzalez, M.D.P., 2020. Depression as a risk factor for dementia and Alzheimer’s disease. Biomedicines, 8(11), pp.457-463.
- Clarke, V. and Braun, V., 2021. Thematic analysis: a practical guide. Thematic Analysis, 3(6), pp.1-100.
- Critical Appraisal Skills Programme (CASP). 2018. CASP qualitative checklist. [online] Available at: https://casp-uk.net/casp-tools-checklists/
- de Oliveira, L.D.S.S.C.B., Souza, E.C., Rodrigues, R.A.S., Fett, C.A. and Piva, A.B., 2019. The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends in psychiatry and psychotherapy, 41(9), pp.36-42.
- Dookhy, J. and Daly, L., 2021. Nurses’ experiences of caring for persons with dementia experiencing responsive behaviours in an acute hospital: A qualitative descriptive study. International journal of older people nursing, 16(4), pp.1-10.
- Flaherty, E. and Bartels, S.J., 2019. Addressing the community‐based geriatric healthcare workforce shortage by leveraging the potential of interprofessional teams. Journal of the American Geriatrics Society, 67(S2), pp. S400-S408.
- Fukuda, R., Shimizu, Y. and Seto, N., 2015. Issues experienced while administering care to patients with dementia in acute care hospitals: A study based on focus group interviews. International journal of qualitative studies on health and well-being, 10(1), pp.1-13.
- Hofmeyer, A. and Taylor, R., 2021. Strategies and resources for nurse leaders to use to lead with empathy and prudence so they understand and address sources of anxiety among nurses practising in the era of COVID‐19. Journal of clinical nursing, 30(1-2), pp.298-305.
- Karaca, A. and Durna, Z., 2019. Patient satisfaction with the quality of nursing care. Nursing open, 6(2), pp.535-545.
- Kelly, L.A., Lefton, C. and Fischer, S.A., 2019. Nurse leader burnout, satisfaction, and work-life balance. JONA: The Journal of Nursing Administration, 49(9), pp.404-410.
- Landeiro, F., Roberts, K., Gray, A.M. and Leal, J., 2019. Delayed hospital discharges of older patients: a systematic review on prevalence and costs. The Gerontologist, 59(2), pp.86-97.
- Mengist, W., Soromessa, T. and Legese, G., 2020. Method for conducting systematic literature review and meta-analysis for environmental science research. MethodsX, 41(9), pp.36-42.
- Molina-Mula, J. and Gallo-Estrada, J., 2020. Impact of nurse-patient relationship on quality of care and patient autonomy in decision-making. International journal of environmental research and public health, 17(3), p.835.
- Palati, S., Ramani, P., Shrelin, H.J., Sukumaran, G., Ramasubramanian, A., Don, K.R., Jayaraj, G. and Santhanam, A., 2020. Knowledge, attitude and practice survey on the perspective of oral lesions and dental health in geriatric patients residing in old age homes. Indian Journal of Dental Research, 31(1), pp.2231.
- Pennbrant, S., Hjorton, C., Nilsson, C. and Karlsson, M., 2020. “The challenge of joining all the pieces together”–Nurses’ experience of palliative care for older people with advanced dementia living in residential aged care units. Journal of clinical nursing, 29(19-20), pp.3835-3846.
- Piirainen, P., Pesonen, H.M., Kyngäs, H. and Elo, S., 2021. Challenging situations and competence of nursing staff in nursing homes for older people with dementia. International journal of older people nursing, 16(5), pp.1-17.
- Sagbakken, M., Spilker, R.S. and Nielsen, T.R., 2018. Dementia and immigrant groups: a qualitative study of challenges related to identifying, assessing, and diagnosing dementia. BMC health services research, 18(7), pp.1-14.
- Şahin, D.S., Özer, Ö. and Yanardağ, M.Z., 2019. Perceived social support, quality of life and satisfaction with life in elderly people. Educational Gerontology, 45(1), pp.69-77.
- Suzuki, H., Venkataraman, A.V., Bai, W., Guitton, F., Guo, Y., Dehghan, A., Matthews, P.M. and Alzheimer’s Disease Neuroimaging Initiative, 2019. Associations of regional brain structural differences with aging, modifiable risk factors for dementia, and cognitive performance. JAMA network open, 2(12), pp.281-289. WHO. 2021. Dementia. World Health Organisation. https://www.who.int/news-room/fact-sheets/detail/dementia